- Proper training is essential when providing Placenta Services to the public!
- Lauren Taylor lives with her 3 children in southern California, in Riverside County. After Lauren experienced placenta encapsulation for herself, with her 3rd baby and 3rd cesarean, she was absolutely amazed at how much faster and easier her recovery was compared to her 2 pervious cesareans. She also didn't experience any of the Postpartum Depression that she had with her previous 2 babies. For Lauren, the effects were life changing, and are what motivated her to pursue Placenta Certification, so that she could help other Moms feel great too!
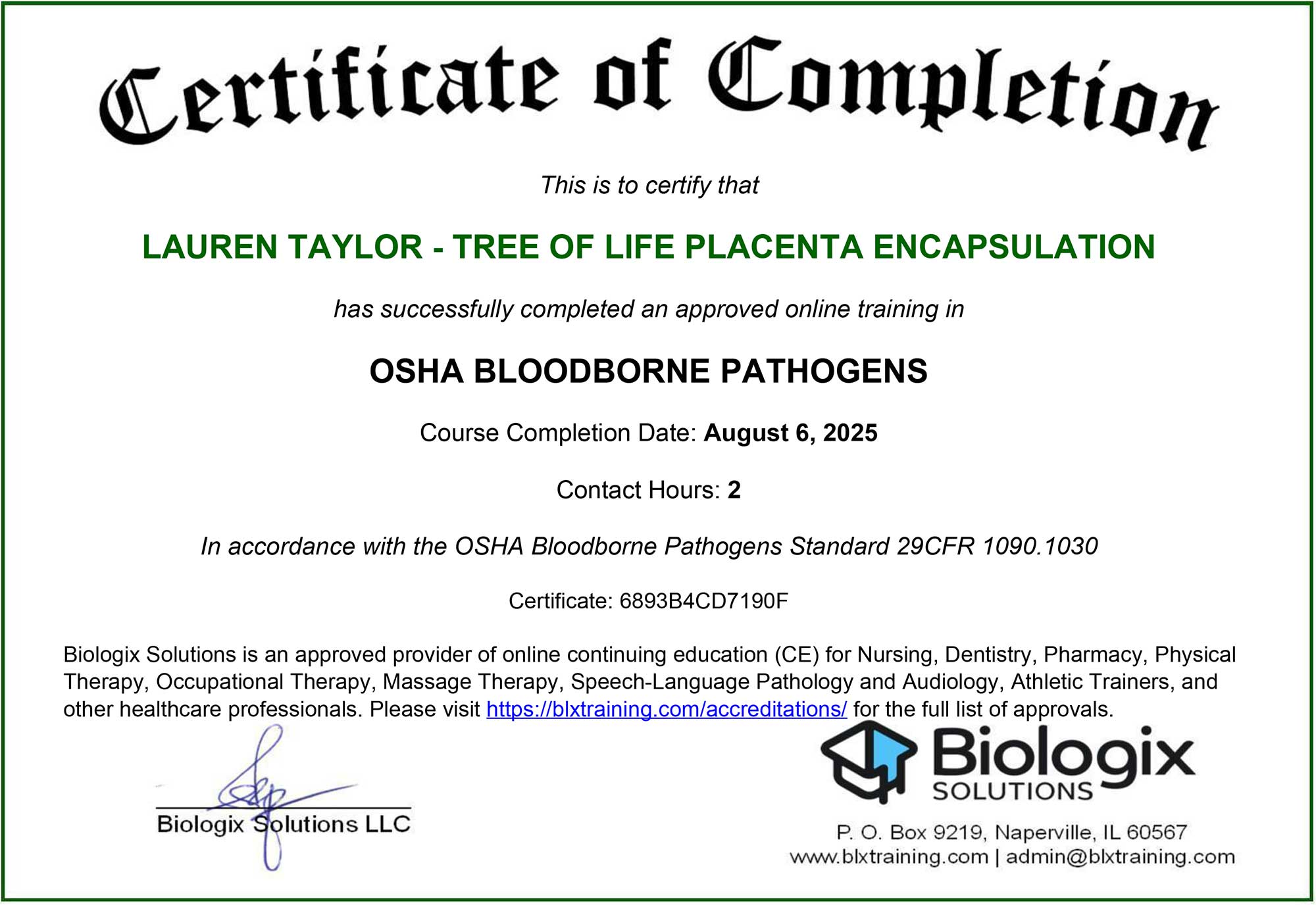
- Lauren has a current "OSHA Bloodborne Pathogens for Placenta Encapsulation Professionals" certificate through Biologix Solutions
- Lauren has a current "ServSafe Texas Food Handler" certificate
- Lauren was Trained & Certified in Placenta Encapsulation through IPPA-International Placenta and Postpartum Association (2013)
- Lauren holds a 2nd Placenta Encapsulation Certificate through BBA-Brilliant Birth Academy (2021)
- Lauren holds a 3rd Placenta Encapsulation Masterclass Certification through Birth Beautifully (2025)
- Non-latex gloves are always worn when Placenta and/or utensils are being handled.
- Anything disposable that has come into contact with blood is disposed of in a red “Biohazard” trash bag for safety.
- Both, before and after Placenta processing, all surfaces and utensils are thoroughly washed with hot water and antibacterial soap…followed by utensils being fully submerged in a Clorox bleach solution and counters being sprayed with same bleach solution and allowing to sit for 10 minutes before a final rinse. This is the standard required by OSHA & the EPA for disinfection and is designed to kill STDs and bloodborne pathogens.
- Anyone handling the placenta must wear protective gloves.
- Any raw organ, such as the Placenta, will colonize bacteria and harbor viruses if not properly handled. This includes transportation and storage of the organ. Thus, proper refrigeration is absolutely crucial. Immediately following delivery, the placenta must be placed into a container or storage bags and put in the refrigerator or a cooler filled with fresh ice.
- The placenta cannot be left out at room temperature for more than 4hrs or it is no longer safe to consume!
- The placenta can be safely refrigerated for up to 4 days - any longer and the placenta should be frozen!
- Some hospitals may require that the placenta be sent to Pathology for testing in certain circumstances (such as: suspected infection or substance abuse, Gestational Diabetes, Chorioamnionitis, Cholestasis, pre-term delivery, retained Placenta, trauma during labor or delivery, and more)
- If the entire Placenta is sent to Pathology then Placenta Encapsulation is no longer safe!
- There are 4 contamination risks when a placenta is sent to a Pathology Lab:
- If the placenta be sent to pathology there is no guarantee the placenta will be kept at the proper temperature of below 41 degrees at all times. This can promote bacterial and viral growth.
- If the placenta is to be sent to pathology your placenta may come in contact with contaminated surfaces and equipment. In many labs the placentas are examined on the same surface as other human tissue or body fluids without proper sterilization between. This means your placenta could come in contact with other people’s bloodborne pathogens.
- If the placenta is sent to pathology your placenta may be exposed to chemicals or preservatives such as formaldehyde.
- If the placenta is sent to pathology, although slight, there is a risk that your placenta could be accidentally switched with someone else’s placenta. There is absolutely no way to be sure you a receiving your placenta back once it has gone to the lab.
- If your placenta must go to Pathology for testing you can request that a piece is cut off and taken separately (have them do this in front of you, never let them take the placenta out of your sight)
- The Hospital does not have the right to take your Placenta - it is a part of the Mother's body, and as such, is her Property!
- Anyone handling placenta products should wash their hands thoroughly afterwards and before touching baby. This is a GBS precaution in case you are Strep B+ at time of delivery but don't know. Group B Strep is very common, found in 10-30% of pregnant women. GBS bacteria come and go naturally in people’s bodies. Therefore, a positive GBS test at 37 weeks does not guarantee that you will be positive at time of delivery, just like a negative test at 37 weeks does not guarantee that you will still be negative at time delivery. If you do test + for GBS then the Hospital will typically administer antibiotics during, and sometimes after, delivery. GBS bacteria is a surface infection and is most commonly spread via skin contact. For this reason, anybody who handles any placenta products of any kind should always wash their hands after handling their placenta products and always before touching baby. GBS bacteria is not transmitted through the GI tract, nor is it passed through breastmilk. Placenta Encapsulation is safe as long as baby, nor placenta, show any signs of infection after delivery. The safest Prep method for those who are concerned about GBS and their newborn's safety is the Gentle Prep method, also known as the Traditional Chinese method.
- Never take more than 6 placenta pills in a 24hr period. Taking too much of your placenta supplement could result in headaches, restlessness, and an oversupply of breastmilk, which could lead to clogged milk ducts or mastitis.
- Never stop taking your placenta supplements abruptly, unless medically necessary. The sudden drop in hormones could cause sudden shifts in mood and energy.
- If sick with infection, like mastitis, or fever of 100.4 or above, stop taking your placenta supplements until you have been on antibiotics or fever-free for 24hrs.
- Always let your Placenta Specialist know if you have: GBS, PUPPS, Chorioamnionitis, Cholestasis, any pregnancy-induced high blood pressure disorders (Hypertension, Toxemia, Preeclampsia, Eclampsia, or HELLP Syndrome), Anxiety, Insomnia, Caffeine Sensitivity, any STI's with active outbreaks during delivery, Gestational Diabetes, or any type of infection or fever (100.4+) during labor & delivery.
- Please let your Placenta Specialist know if your baby has any of the following genetic conditions: Cerebral Palsy, Cystic Fibrosis, Sickle Cell, Tay-Sachs, or Thalassemia.
Lauren Taylor is dedicated to helping the new moms of Southern California have a better postpartum recovery!